In the realm of neurological disorders, some conditions remain obscured in the shadows despite their devastating impact. Cluster headaches—aptly nicknamed “suicide headaches”—represent one such affliction that deserves significantly more attention from the medical community and public awareness.
Author: Teresa Jardim
Cluster Headaches, also known as Horton’s Syndrome, are a rare neurological disease that affects less than 1% of the population. Nonetheless, it can develop at any point in one’s life and affect anyone. Research surrounding Cluster headaches is extremely reduced and rarely accessible; awareness regarding the disease is thus essential.
The best way to comprehend such a condition, is by listening to people who have lived with Cluster Headaches. Domincian Paten – a 25-year-old man who has been diagnosed for around 7 years – can better explain the reality of living with such a disease.
The Interview
He was “diagnosed when [he] was 18, although the first symptoms appeared when [he] was 15 or 16.”
Although living with such a disease is not easy, the diagnosis does not facilitate the patient’s condition.
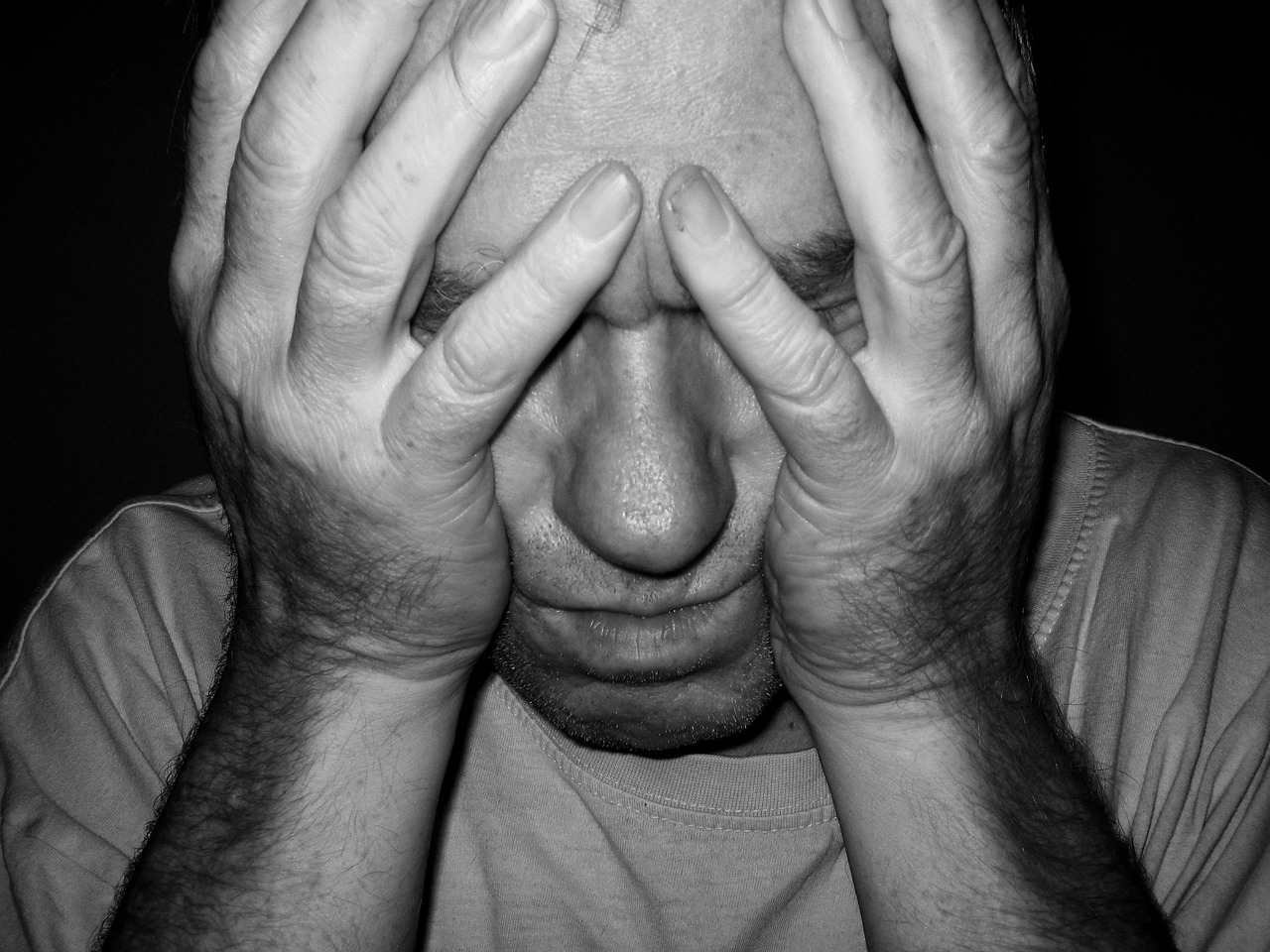
Although misleading by name, cluster headaches are not in any way comparable to a normal primary headache disorder (migraines and tension headaches). Indeed, migraine disorders are often characterized by intense pains, light and sound sensitivity, and can be accompanied by nausea and vomiting. However, cluster headaches are considered by neurologists to be 100 times worse, and patients even go as far as saying that they are comparable to an amputation made with no anesthesia. This is why they are called “suicide headaches”, a name that fits reality.
Q: “Do you think “suicide migraines” describes the reality of living cluster headache well?”
A: “Yes, totally, I wouldn’t wish it on anyone. You aren’t exactly lucid during the crisis, and when you are tortured by your body for hours, during four to six times a day, and that you know it will happen again, of course you have some dark thoughts… Several people have committed or attempted suicide because of it.”
An individual who is diagnosed with Horton’s Syndrome can episodic or chronic. The episodic type, which can last between 7 days to one month, followed by a remission which can last from 3 months to a year. Once the chronic version of the illness, is developed, the individual will continue to have episodes of the disease for the rest of their lives with usually no pattern of remissions.
An individual who suffers from this will have unilateral bouts of pain which can affect the suborbital and orbital-temporal regions of the face, as the pain is usually described as affecting mostly the regions around one eye as well as the neck and jaw.
Q: “How do you physically react during a crisis?”
A: “It’s often on my right side, as I have a chronic unilateral right-sided condition. My right nostril is runny, my eye gets watery, the whole right side of my face gets swollen. I become rapidly agitated; I move around a lot to find a more comfortable position that is less painful. Sometimes I scream from pain or bang my head against the floor.”
The bouts of pain caused by Horton’s syndrome are not linear, as they are usually divided into three different phases.
- The first phase of an episode is referred to as the preictal phase. This is when early symptoms start to appear, it usually lasts 10-60 minutes and is typically characterized by difficulties concentrating, restlessness, and even a dull pain around or behind the eye.
- The ictal phase is when pain reaches the highest and the most symptoms are experienced. Around 4 symptoms are usually experienced, the most common being (alongside with orbital-temporal pain), lacrimation and conjunctival injection. This phase usually lasts between 1-2 hours and can happen around 1-4 times a day. During this phase, individuals experience intense restlessness and intense psychological turmoil as well.
- The third and final phase is the postictal phase. As it is usually more dependent on the individual and their respective treatment,
As of now there is no known cure, but there are multiple medications to help reduce the hardships experienced during the periods of pain.
Q: What are the viable options to ease the pain?
A: “For crisis treatment: oxygen therapy and the use of triptans [either by injection or nasal spray]. For preventive treatment: emgality once or twice a month, morphine, ketamine perfusion at a pain center. But the preventive treatments rarely work on pharmacologically resistant [an individual with high drug tolerance] individuals, like me…”
Different medications help with different effects. For instance, Triptane is used for contracting the dilated veins in the brain, emgality [or galcanezumabe] is a medication specifically made for helping patients of cluster headaches, and morphine or ketamine are used as painkillers to try and reduce the levels of pain. Other options include seizure medication such as Divalproex and Topiramato and mood stabilizers such as lithium medication.
Scientifically, there are no concise answers as to the mechanisms of a pain bout. This is because all the studies use animal models to map the neuroanatomical pathways, as the nature of the human brain is complex, and the essence of the attacks remains unkonwn.
Recent progresses have helped develop three possibilities for causes of the disease, based on three different neuroanatomical structures.
The first possibility is the altered activation of the trigeminovascular pathway activation. This is a possibility for explaining the location of the pain as being around the beginning of the trigeminal nerve. The altered activation of this pathway can lead to the release of CGRP and PACAP-38 (both of which are neuropeptides). These neuropeptides have been proven to pharmacologically induce cluster headaches, and they influence blood vessel dilation and inflammation. That is part of the reason why triptans ( who block the transmission of the neuropeptides and help reduce inflammation), are good at helping to deal with periods of crisis.
The second possibility suggested, is the activation of trigeminal-automatic reflexes. The trigeminal automatic reflexes is composed of neurons originating in the trigemino-cervical complex (connects facial and neck pain pathways). These will also activate the nasal and lacrimal glands therefore causing symptoms like lacrimation. Simultaneously, the activation of this reflex prompts the release of neuropeptides including PACAP-38.
While it is proven that the trigeminal-automatic reflex cannot cause the bouts themselves, they can cause symptoms and start a cycle with the trigeminovascular pathway, causing more pain.
The third and final possible explanation given is the involvement of the hypothalamus. In neuroimaging studies there has been a link between the size of the inferior hypothalamus compared to the superior hypothalamus in people with more regular crisis. The connection of the hypothalamus with the medial frontal gyrus (part of the frontal lobe) and with the occipital cuneus (part of the occipital lobe). Increased signaling in the connection between the hypothalamus and the MFG is linked with intensity of pain during a normal migraine, and the occipital cuneus is linked with light sensitivity also during migraines.
In view of this there is a possible link between the hypothalamus structure and cluster headaches. It is important to note that the Hypothalamus is connected to both the trigeminovascular pathway and the trigeminal-automatic reflexes, therefore the cause of pain may not be one of the three possibilities but can stem from a connections or a cycle of all three of the explanations above.
Living with a disease like this can reduce your quality of life, make it harder to navigate small tasks, and often leads to trouble finding or keeping a job.
Q: Do substances like tobacco or alcohol affect the crisis?
A: “Of course, you should avoid those substances, as well as strong smells, salty foods, etc.”
Q: How do the different seasons affect the frequency of the crisis?
A: “Cold or very hot weather can trigger a crisis, as well as strong lightning: I can’t leave the house without sunglasses.”
Q: How did this condition affect the course of your life?
IA: “It ruined it. I had to stop my studies, exercising, work. It’s also hard for my partner/girlfriend to see me suffer every day without being able to help.”
The development of Horton’s syndrome is yet to be fully grasped. Nonetheless, it has been found that the disease is linked with genetics; if someone in your close family has Horton’s syndrome, you are 5-18 times likelier to develop it.
Other than this, there are no known and evident causes of the disease, and there are not a lot of extensive studies done on the subject, and even less ones that are accessible and easy to comprehend. Due to the rarity and complexity of Cluster Headaches, scientists do not have a lot to work with.
Q: Do you believe that doctors and the healthcare system are equipped to help individuals with conditions such as cluster headaches?
A: “It could be, but there aren’t enough studies done on the subject, the brain is pretty complex…”
The most important topic concerning a disease such as this one is awareness and support. In Belgium, “Unlike other conditions, cluster headaches are recognized by the Vierge Noire [the Belgian handicap association], which is nice. On the psychological side, there are support groups where you can share your experience and ask questions and advice.”
Awareness surrounding diseases such as Horton’s Syndrome, is essential to help expand the research conducted. As scientists better understand the brain and its mechanisms, treatments advance and people can be saved from the troubles of living with suicide headaches.
Editor: Olivia Pataki